Treatments
Congenital malformations




Congenital malformations require an individualized approach, considering age, growth potential, and function. The therapeutic plan combines physiotherapy, orthotics, and, when indicated, staged reconstructive surgery. Techniques include epiphysiodesis for growth control, gradual bone lengthening with an external fixator or motorized rod, tendon transfers, targeted osteotomies, and joint reconstruction. In longitudinal deficiencies, segments can be realigned, the hip/knee/ankle can be stabilized through joint reconstruction techniques such as Superhip, Superknee, Superankle, and plantar support can be optimized. The goal is to align, equalize lengths, and improve gait, preserving as much native tissue as possible and respecting developmental milestones.
Bone dysplasias




Bone dysplasias are alterations in bone growth and structure that can cause deformities, shortening of the upper and lower limbs, and limitations in function and aesthetics. In more severe cases, the bone grows crooked or weakened, requiring specialized treatment. The bone reconstruction method is the main option in these cases. It uses external fixators, such as the Ilizarov or TL-Hex, or internal implants that allow for the correction of deformities and the lengthening of the bone gradually and safely. After a controlled cut (corticotomy), the bone is separated millimeter by millimeter, and the body forms new bone tissue between the parts, restoring alignment and natural length. An example is focal fibrocartilaginous dysplasia, in which part of the bone is replaced by fibrocartilaginous tissue, causing progressive curvature and shortening. Treatment with bone reconstruction allows for realignment of the limb, restoration of length, and improvement of function. The ultimate goal is to re-establish form, balance, and movement, giving the patient a better quality of life.
771 different entities associated with 552 genes have already been cataloged. Genetic skeletal dysplasias represent a broad and growing spectrum of conditions that primarily affect growth cartilage, bone, ligaments, and joints — according to the 11th revision of Nosology of Genetic Skeletal Disorders: 2023 Revision. Although most cases involve mutations in genes that regulate endochondral growth, bone morphogenesis, and the extracellular matrix (for example, mutations in the FGFR3 or COL2A1 gene, responsible for classic bone shortening dysplasias), there is also a relevant subpopulation of growth failures caused by endocrine factors — such as growth hormone deficiency, GH/IGF-1 resistance, or thyroid dysfunction — and systemic diseases (such as metabolic or storage diseases) that secondarily interfere with skeletal development. Understanding the genetic, endocrine, or other mechanism of etiology (e.g., lysosomal storage, hormonal excess, altered bone metabolism) becomes fundamental for the orthopedist, endocrinologist, and reconstructive surgeon, since treatment, prognosis, and follow-up differ widely depending on the underlying mechanism—and the simple term "dwarfism" or "limb shortening" can encompass radiologically, genetically, and functionally very distinct conditions.
Achondroplasia





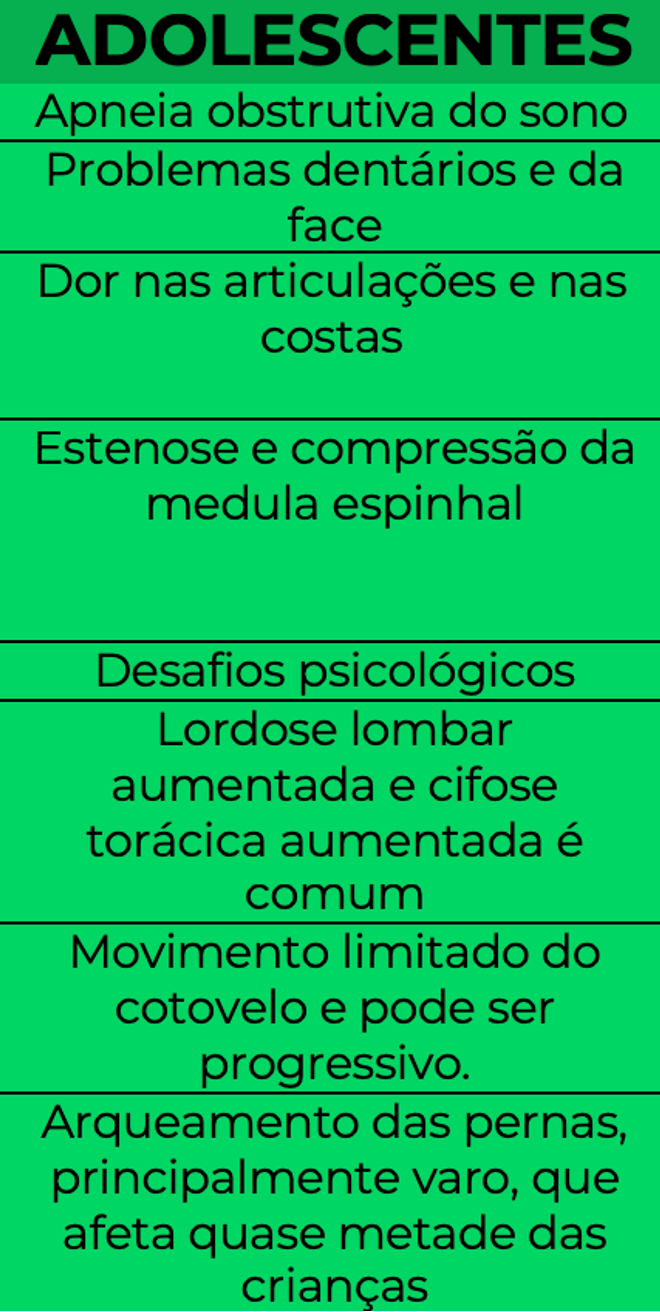



Achondroplasia is the most common dysplasia and a genetic condition that causes changes in the growth of long bones, resulting in short stature and shortened limbs, but preserved intellectual development. Deformities and limitations in gait and upper limbs may occur. Treatment can be medical and surgical, depending on age and severity. There are already medications such as vosoritide, which act directly on bone growth, stimulating the lengthening of growth plates and reducing the rate of deformities in children. In cases with more pronounced shortening or already established deformities, surgical treatment is the most indicated. Options include the bone reconstruction method with external fixators (such as monolateral and hexapodal) or the use of motorized intraosseous lengthening rods, which allow the bone to be lengthened in a controlled and discreet manner, without visible external structure. Both methods use the biological principle of osteogenic distraction, in which the bone is gradually separated after an osteotomy, forming new bone tissue. The goal of treatment is to improve body proportions, correct deformities, and enhance limb function, leading to greater independence and quality of life.
Osteometabolic diseases




Diseases such as rickets, osteogenesis imperfecta, osteomalacia, hormonal disorders, and renal osteodystrophy alter bone quality and axis. Care integrates clinical treatment (correction of calcium, phosphorus, vitamin D, bisphosphonates when indicated) and surgery. Mechanical axis-guided osteotomies, telescopic intramedullary implants in pediatrics, and external fixation for gradual corrections are frequent resources. Planning considers bone age, active physes, and risk of refractures. Physical therapy, pain control, and supplementation support consolidation. The goal is to align, reduce pain, and improve gait, balancing mechanical stability with optimized bone metabolism.
Aesthetic bone lengthening


Esta ilustração tem caráter exclusivamente informativo e não representa resultados individuais. O procedimento deve ser indicado e acompanhado por médico especialista.
Aesthetic lengthening is indicated after careful evaluation, emotional stability, and understanding of the risks. The planning defines realistic goals (generally 5–8 cm) per segment, distraction rate, and biomechanical impact. Motorized intramedullary rods or external fixators with gradual distraction are used, respecting 1 mm/day in fractions. Intensive physiotherapy prevents contractures and maintains alignment. Nutritional supplementation, pain control, and radiographic monitoring ensure quality regeneration. The decision is shared and requires strict adherence; possible complications include delayed consolidation, stiffness, neuropathic pain, and patellofemoral imbalances, which are monitored and treated early.
Arthroplasty in amputees (osseointegration)



Osseointegration is a surgical technique that directly fixes a metal implant to the residual bone, connecting it to the prosthesis without the need for a socket. The goal of the procedure is to restore the anatomical and functional connection between the skeleton and the prosthetic component, offering greater comfort, motor control, and natural proprioceptive sensation (osseoperception). The surgery takes place in two stages: in the first, the bone canal is prepared and the implant is inserted; in the second, after bone integration, the percutaneous connector that links the implant to the external prosthesis is attached. It is indicated for patients with pain when using the socket, sensitive skin, or difficulty lifting the prosthesis. Benefits include improved control and mobility, reduced skin irritation, and greater naturalness in movements. Risks include infection along the skin tract, loosening of the implant, and fractures of the residual bone. Rehabilitation is gradual and focuses on training axial load, balance, and functional adaptation.
Brachymetatarsia and foot dysplasias




Brachymetatarsia causes metatarsal shortening, overload, and aesthetic/functional discomfort. Management can be conservative with insoles and appropriate footwear, but symptomatic cases indicate metatarsal lengthening. Techniques include osteotomy with intercalary graft and fixation, or gradual lengthening with a mini-external fixator, allowing controlled gains and soft tissue adaptation. In associated dysplasias, hindfoot/forefoot alignment is assessed and concomitant deformities are corrected. Careful planning of plantar length and arch aims to distribute loads, relieve pain, and improve footwear use and aesthetics, with rehabilitation and progressive return.
Congenital or syndromic clubfoot




Standard treatment for idiopathic congenital clubfoot begins with the Ponseti protocol: serial manipulations, weekly casts, and Achilles tenotomy when necessary, followed by orthotics for maintenance. In syndromic or rigid cases, posteromedial releases, osteotomies, or gradual corrections with a hexapodal external fixator for three-dimensional alignment may be necessary. The goal is to achieve a plantigrade, painless, and functional foot, preserving mobility. Adherence to orthotics is crucial to prevent recurrence. Physical therapy, gait monitoring, and orthopedic adjustments to growth complete the longitudinal care of the child.
Joint stiffness and contractures


Joint stiffness results from prolonged immobilization, persistent pain, capsular fibrosis, and musculotendinous imbalances, causing loss of movement and mechanical pain. Acquired causes involve rheumatological diseases (rheumatoid arthritis, psoriatic arthritis), infectious or traumatic synovitis, metabolic diseases (diabetes, gout), sequelae of fractures, surgeries, and prolonged immobilization. Congenital forms, such as congenital multiple arthrogryposis, result from musculoskeletal anomalies with stiffness and contractures from birth. Treatment includes targeted physiotherapy, analgesia, and dynamic orthoses. If limitations persist, arthroscopic releases, tendon lengthening, capsulotomies, or joint fixators are indicated. Intensive rehabilitation and manual therapy promote functional gain. Surgical timing respects healing and functional goals, seeking to recover useful and painless mobility, preventing recurrence with home exercises and a gradual return to activities.
Lesions associated with infection and osteomyelitis

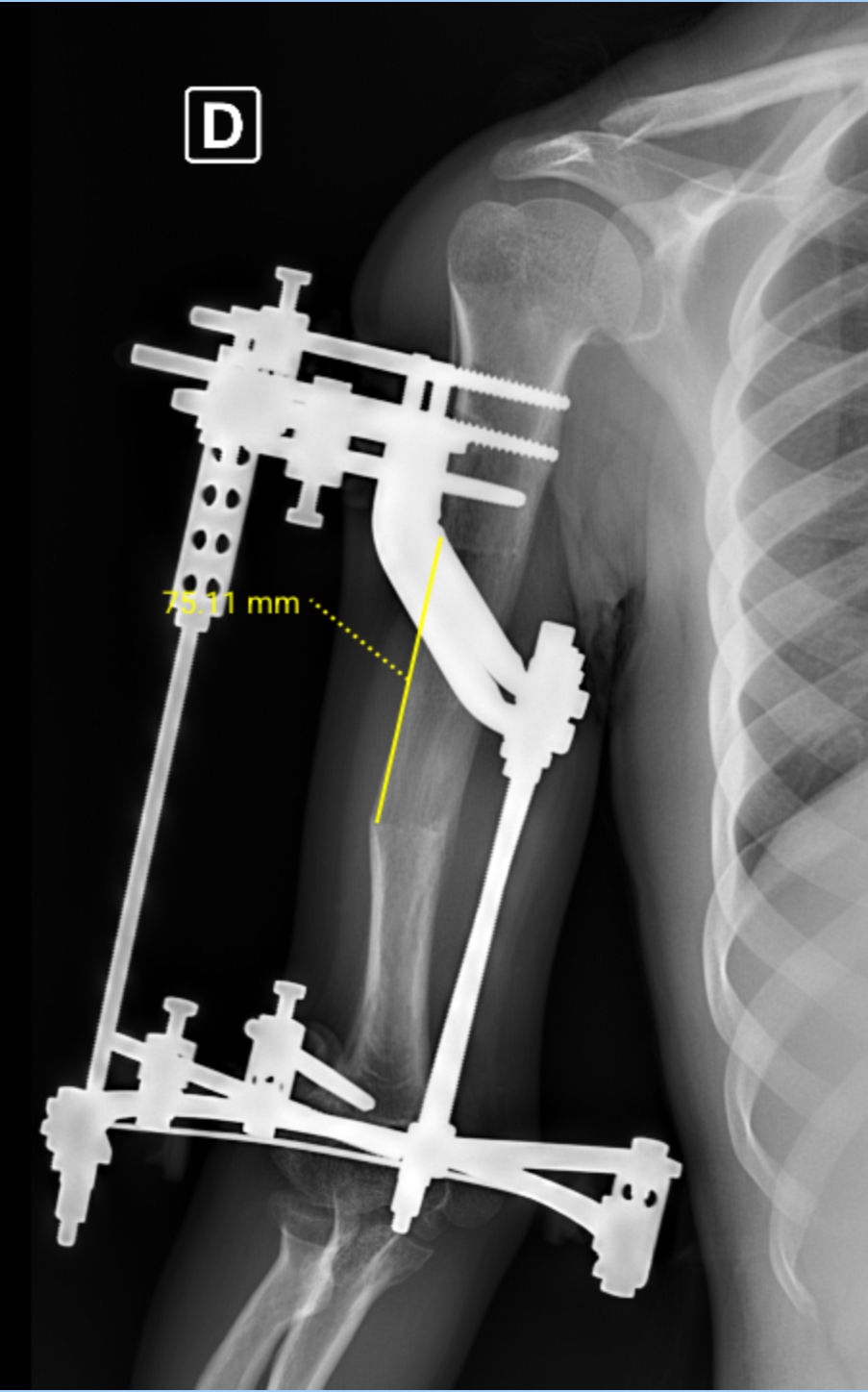
Quebra de implantes


Quebra de implantes
The management of osteomyelitis requires infection control and sequential reconstruction. Treatment includes extensive debridement, targeted cultures, guided antibiotic therapy, stabilization with an external fixator, and cavity filling with temporary spacers such as methyl methacrylate or calcium sulfate cement with local antibiotics, permanent spacers such as bioglass, or Masquelet-type techniques. When segmental defects are present, bone transport is performed using the Ilizarov method or autologous structural grafts. Soft tissue coverage may require flaps. Treatment is phased: eradicate infection, stabilize, reconstruct bone, and restore function. Dressing protocols, laboratory monitoring, and monitored rehabilitation reduce recurrence and promote stable consolidation with progressive weight-bearing.
Non-union fractures (pseudoarthrosis)

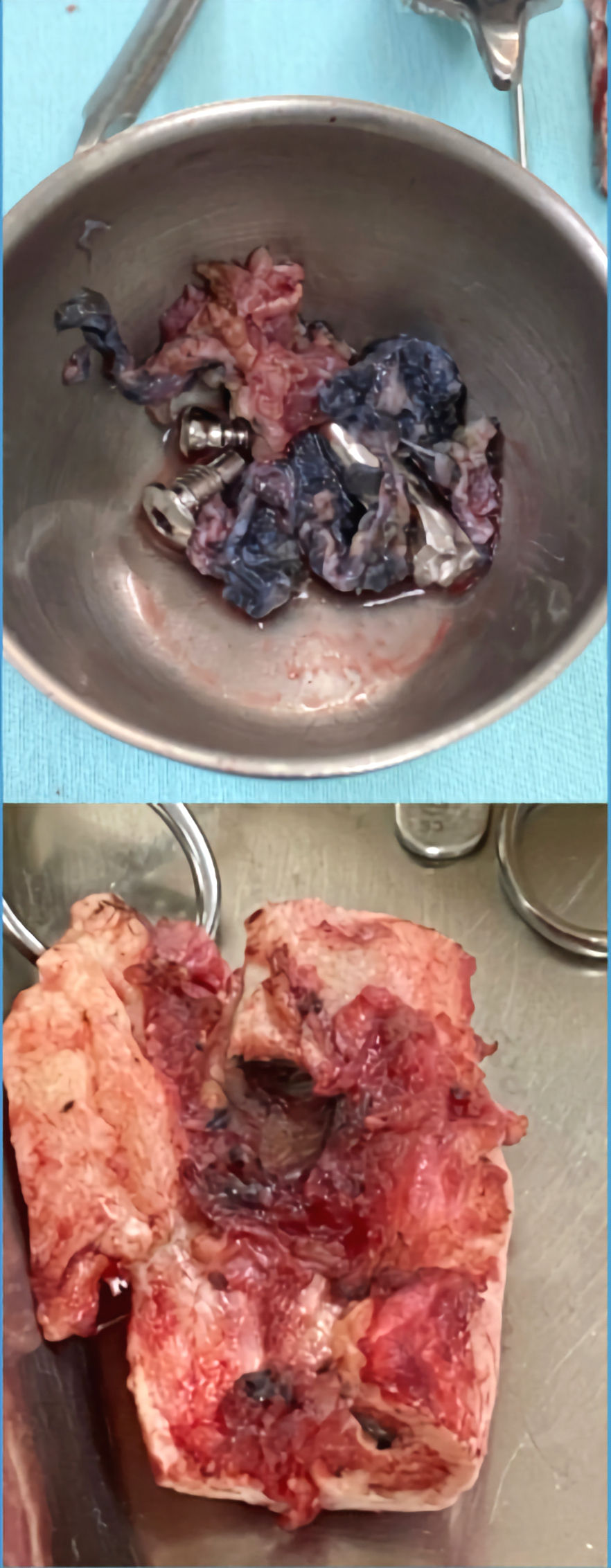
Quebra do implante de fixação prévio



Quebra do implante de fixação prévio
Among the most challenging conditions in orthopedics, pseudoarthrosis is always among the most frequently cited by specialists. Chronic infection, residual deformities, bone sclerosis at the focus, osteopenia, joint stiffness, and long treatment times are just some of the complications that generate serious psychological, social, and economic implications for patients who have it. It requires identifying the causes: instability, biological deficiency, infection, or misalignment. Treatment combines rigid stabilization (locked plates, intramedullary nail, or external fixator), axis correction, and biological stimulation with autologous or synthetic grafts. In segmental losses, bone transport by Ilizarov or Masquelet technique are options. Smoking, nutrition, and metabolism are evaluated. Electrical and ultrasonic stimulation can be helpful. The goal is to consolidate with good alignment and function, reducing pain and restoring gait.
Complex fractures with soft tissue injury




In high-energy fractures, "damage control" is prioritized: temporary stabilization with an external fixator, soft tissue protection, and delayed planning for definitive fixation. Computed tomography (CT) scans aid in fracture mapping. Options include locking plates, intramedullary nails, and, when necessary, a circular fixator for gradual alignment. Skin and muscle injuries guide surgical timing and, if needed, flaps for coverage. Infection prophylaxis, analgesia, anticoagulation, and early physiotherapy prevent complications. The goal is to achieve anatomical consolidation with preserved function, respecting bone biology and the priority of soft tissue care.
Inveterate and complex deformities
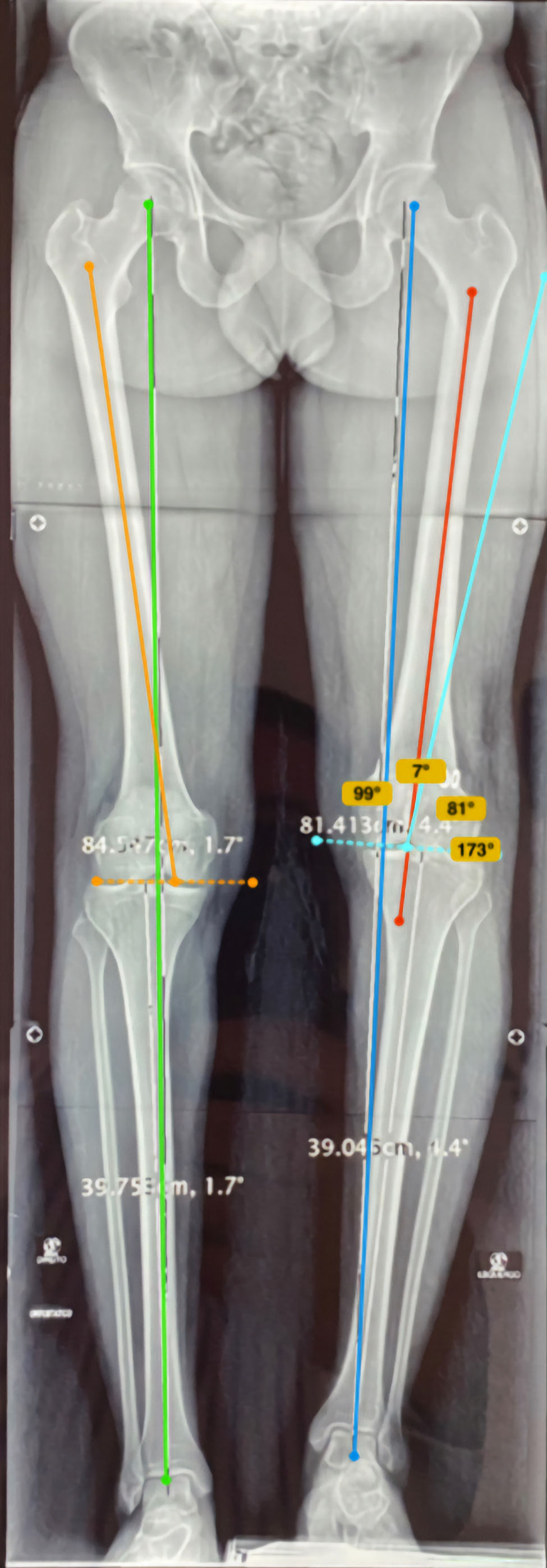


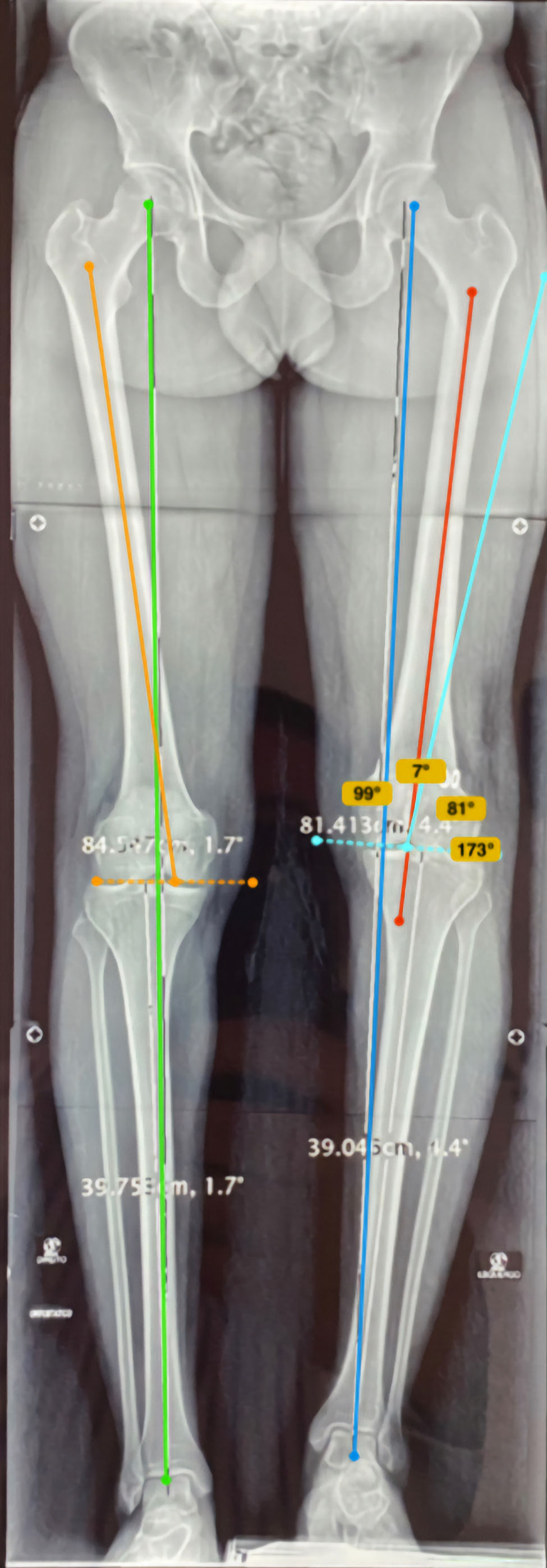
Chronic deformities combine multiplanar deviations, shortening, rotation, and joint stiffness. Treatment begins with 3D mapping, mechanical axis study, and evaluation of soft tissues, nerves, and vessels. Multiplanar osteotomies are employed, followed by gradual correction with conventional circular external fixators, monolateral external fixators, and modern fixators assisted by dedicated software for millimeter adjustments, or acute correction with plates/rods when soft tissues allow. Structural grafts or bioactive substitutes assist in bone loss. In cases with stiffness, capsular release and muscle lengthening are added. The focus is on restoring alignment, function, and painless weight-bearing, with intensive rehabilitation and serial radiographic monitoring.
Post-traumatic deformities



Correção final

Post-traumatic deformities result from malunion, bone loss, ligamentous injuries, and residual asymmetries. Treatment begins with clinical and three-dimensional radiographic analysis, evaluation of mechanical axis, rotation, and length, as well as the condition of the soft tissues. Options include percutaneous or open corrective osteotomies, stabilization with a circular external fixator (Ilizarov method) or intramedullary plates/rods, possibly associated with bone grafting or substitutes. Navigation using digital planning and 3D-printed guides increases precision. Early rehabilitation and gradual adjustments allow for the correction of angulation, rotation, and shortening with functional safety.
Salvage Arthrodesis



Post-traumatic deformities result from malunion, bone loss, ligamentous injuries, and residual asymmetries. Treatment begins with clinical and three-dimensional radiographic analysis, evaluation of mechanical axis, rotation, and length, as well as the condition of the soft tissues. Options include percutaneous or open corrective osteotomies, stabilization with a circular external fixator (Ilizarov method) or intramedullary plates/rods, possibly associated with bone grafting or substitutes. Navigation using digital planning and 3D-printed guides increases precision. Early rehabilitation and gradual adjustments allow for the correction of angulation, rotation, and shortening with functional safety.
Treatments
Bone lengthening technique with external fixator over intramedullary nail (LON)

What is LON?
It is a lengthening technique that combines, in the same treatment, an external fixator (for a short period) and an intramedullary nail locked inside the bone. The idea is to use the fixator only to gradually "open" the bone (distraction) and use the rod to stabilize the limb during and after lengthening, shortening the time with pins and arches in the skin. Studies and reviews indicate that LON reduces the time of external fixation and improves axis control compared to the use of the external fixator alone.
Why can bone lengthen?
Lengthening takes advantage of the bone's natural ability to form new bone when the two halves are slowly separated after an osteotomy (controlled surgical cut). This principle – called osteogenic distraction – is the basis of all modern lengthening methods.
Step-by-step of LON
See the steps Planning and case selection 1. Clinical and radiological evaluation, planning of the axis and amount of lengthening; discussion of goals, risks, and rehabilitation. 2. Surgery – initial phase – A corticotomy (osteotomy) is performed at a planned location. – A locked intramedullary rod is introduced into the bone canal (femur or tibia). – An external fixator (e.g., Ilizarov or LRS) is mounted with the percutaneous pins positioned outside the path of the rod. This simultaneous combination is called "hybrid fixation". 3. Latency (onset of healing) – Short period after surgery (typically ~1 week) before distraction begins, allowing for initial callus formation. 4. Distraction (the actual "stretching") – The patient/team performs programmed rotations on the external fixator, several times a day, to separate the bone halves at a slow and constant rate (in classic protocols, approximately ~1 mm/day, adjusted to age, bone type, and regenerated bone quality). – Active physiotherapy from the beginning to maintain mobility and stretch muscles/tissues. 5. Removal of the external fixator and consolidation with the rod – When the planned length is reached and the new bone is progressing well, the external fixator is removed. – The rod is locked with new screws and continues to provide internal stability while the bone "matures" and calcifies until it is completely consolidated. This greatly reduces the period with pins in the skin.




Motorized internal intramedullary nail bone lengthening technique (ILN)

What is the ILN technique?
Motorized nail bone lengthening represents an evolution of the Ilizarov method — applying the same biological principles, but with internal technology and superior comfort.
Intramedullary motorized nail bone lengthening is a modern orthopedic reconstruction technique that allows increasing the length of the bone (usually femur or tibia) internally, without a visible external fixator.
The nail is implanted inside the medullary canal of the bone and has a motorized electronic mechanism, controlled by an external radiofrequency (RF) or magnet system, which promotes progressive and precise lengthening.
Operating principle
The Ilizarov method continues here: controlled osteotomy + gradual distraction → formation of new (regenerated) bone in the created space.
The difference is the internal distraction mechanism, which replaces the use of external fixators.
Main Orthopedic Indications
Lower limb length discrepancy (>2 cm)
Congenital shortening (mild congenital malformations and mild bone dysplasias)
Post-fracture or infection sequelae (consolidated pseudoarthrosis with shortening)
Aesthetic lengthening (selected cases and under strict supervision)
Limited correction of associated deformities (when the axis allows intramedullary correction)
Main Advantages
No external fixator required (better comfort and aesthetics)
Lower risk of pin tract infection
Less pain and greater freedom for the patient
Faster return to daily activities
Contraindications and Limitations
Active or recent bone infection
Very narrow medullary canal (technical impossibility of implantation)
Complex angular distortions → prefer circular external fixators (Ilizarov/hexapodal)
Severe osteopenia, metabolic disorders Bone problems
Lack of adherence to or understanding of the protocol (the patient needs to follow the distraction program diligently)
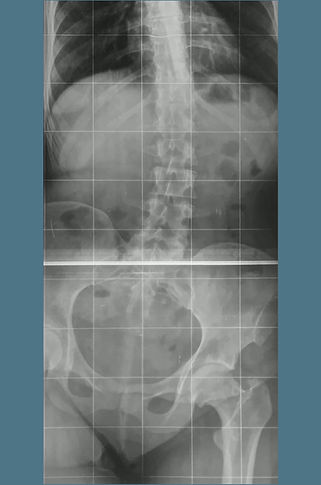
Step-by-step of the ILN
See the steps 1️⃣ Preoperative planning - Panoramic radiographs and tomography to measure the limb and plan the axis. - Choice of rod model and length. - Definition of the osteotomy zone and lengthening target. 2️⃣ Surgery - Performed under anesthesia, with the patient in the supine position. - Introduction of the motorized rod into the medullary canal after reaming. - Minimally invasive osteotomy (metaphyseal, preserving the periosteum). - Fixation of the rod with proximal and distal screws. - Testing of the internal motor function with the external control. 3️⃣ Immediate postoperative period - Physiotherapy and partial ambulation initiated early. - The patient performs the stretching under medical guidance. 4️⃣ Distraction phase (stretching) - Start after 5–7 days of latency. - Activation with external control: 0.25 mm × 4/day = 1 mm/day. - Weekly radiographs to monitor regeneration and alignment. - Duration: approximately 10 days per desired centimeter (e.g., 5 cm → ~50 days). 5️⃣ Consolidation Phase - Distraction is discontinued after reaching the planned length. - The new bone gradually mineralizes. - Progressive partial weight-bearing according to radiographic density. - Monthly radiographs until consolidation (≈ 1–2 months/cm lengthened). 6️⃣ Rehabilitation - Daily physiotherapy: joint mobility, strength, and gait. - Full weight-bearing and return to activities generally between 6 and 12 months. 7️⃣ Rod Removal After complete consolidation and length stability. Elective, minimally invasive procedure under anesthesia.